Hip Fracture Rates - Positive Impact in Ontario
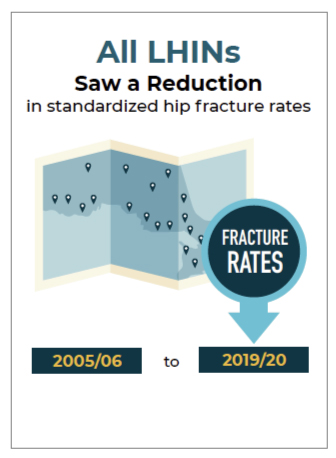
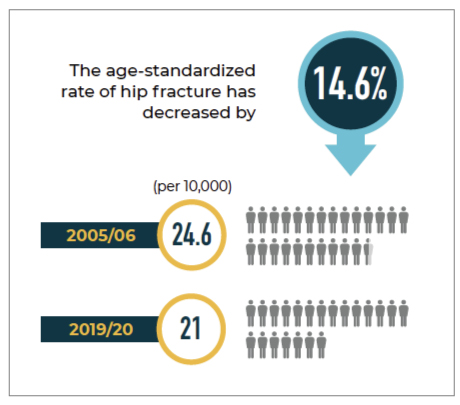
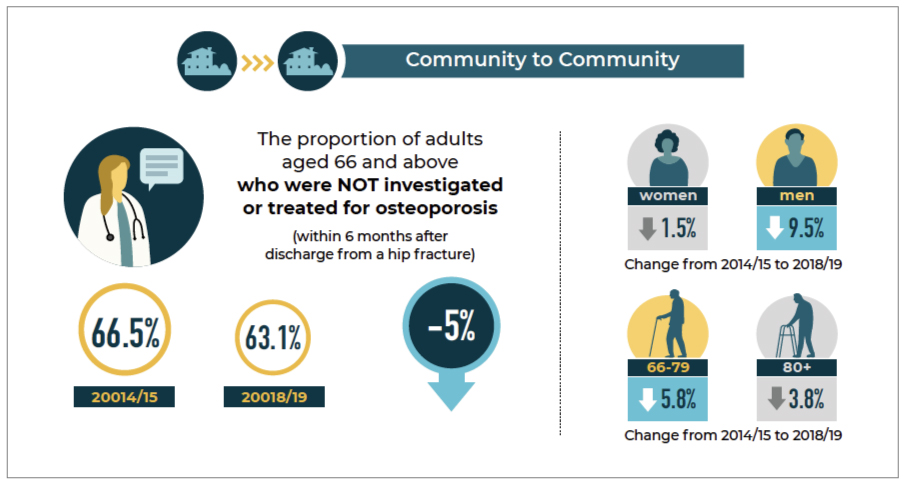
The Ontario Osteoporosis Strategy has achieved a significant and positive trend in hip fracture prevention, boasting a notable 14.6% decrease in the age-standardized rate of hip fractures over the past 15 years, indicative of substantial advancements in healthcare and prevention initiatives for all age groups and genders.
Report Overview:
This report offers updated data on fracture rates, BMD testing, and osteoporosis treatment indicators in Ontario. New indicators, with a focus on Long-Term Care (LTC) residents, are included. Note that this report replaces previous Ontario Osteoporosis Program Reports and incorporates methodological refinements, medication updates, and emphasis on trends in hip fractures, fracture rates among seniors aged 80+, LTC settings, and variations across Local Health Integration Networks.
Evaluation Objectives:
1. Analyze trends in fracture rates, bone mineral density (BMD) testing, and osteoporosis treatment in Ontario from 2005/06 through 2019/20.
2. Provide insights to guide the ongoing and future direction of the Osteoporosis Program.
HIp Fracture Rates
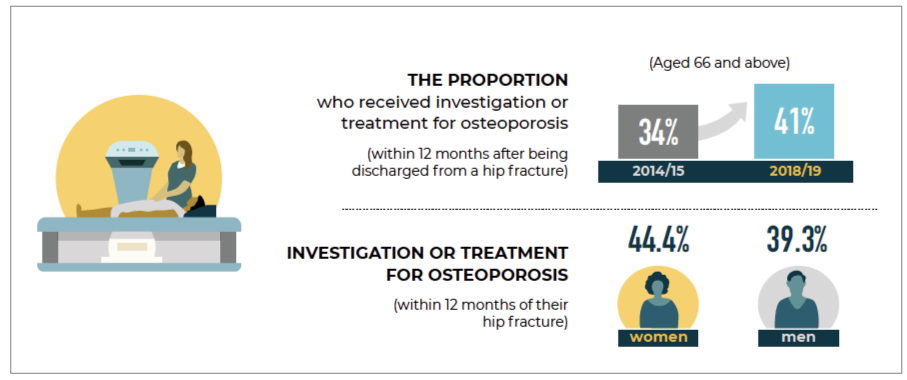
BMD Testing and/or Treatment
Residents in LTC are at very high risk for fracture and need individualized treatment. Care
needs to be patient centred and individualized based on goals of care and life expectancy.
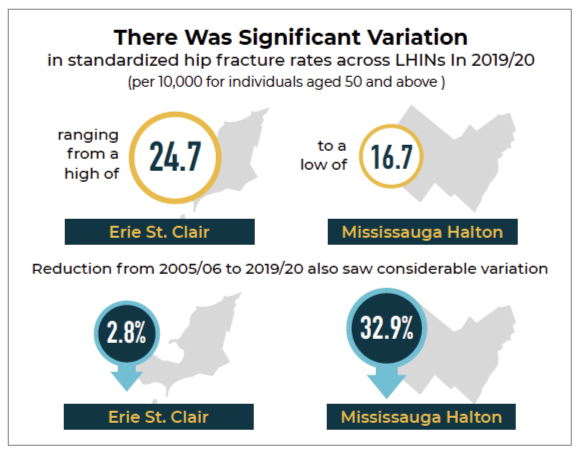
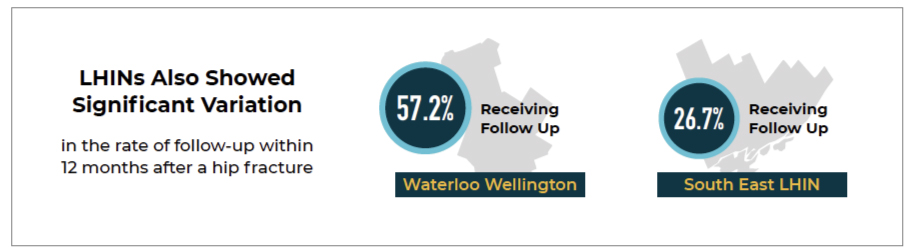
In 2019/20, the standardized hip fracture rates (per 10,000) for individuals aged 50 and above ranged from 24.7 in Erie St. Clair to 16.7 in Mississauga Halton. This indicates a significant variation in hip fracture rates across different Local Health Integration Networks (LHINs) and highlights the need for further investigation and analysis across various indicators.
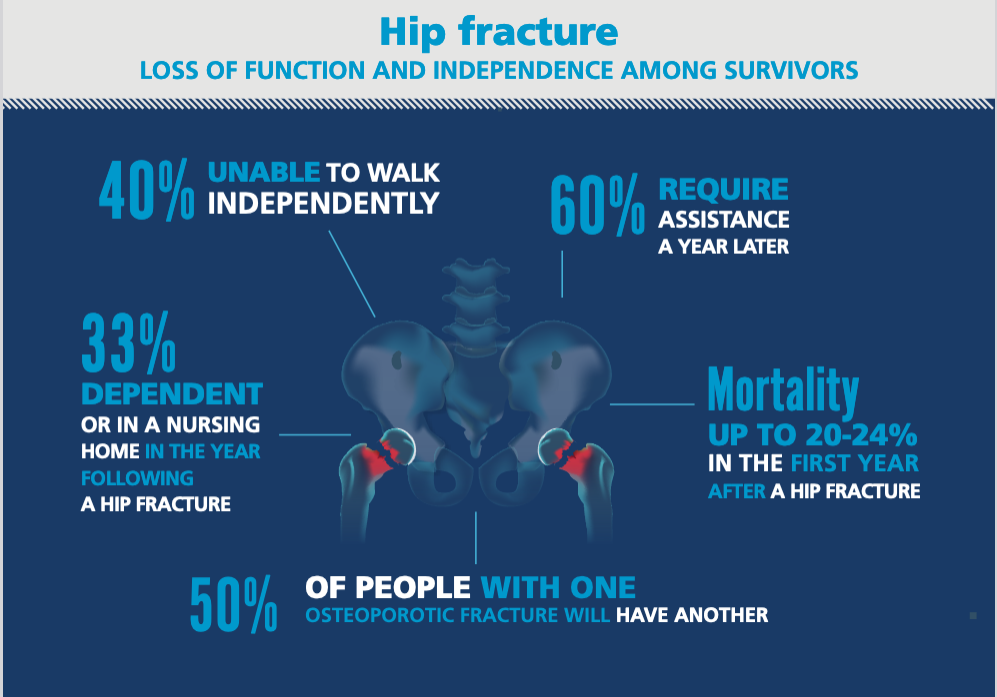
Despite the high risk of fractures in males, they continue to be undertreated compared to females, contributing to significant health system utilization and costs associated with hip fractures.