Fracture Link Newsletter
Volume 2
A continuous effort
What began as a very unique program in Canada and throughout the world has started a movement of change around the world. The Ontario Osteoporosis Strategy continues to move along with emerging trends in research and now influencing the formation of various fracture reduction strategies around the world. This, our second newsletter, highlights the critical research efforts underway in Ontario and the passion of one champion in the pursuit of fracture reduction in Canada.
The Fracture Clinic Screening Program (FCSP) research and evaluation team continues to engage in knowledge translation and promotion of the FCSP on a national and international level by publishing findings in peer-reviewed scientific journals. The first two published manuscripts using data obtained through the FCSP focused on the role of patient perceptions. The FCSP is one of the only databases in the world that routinely collects data on patient perceptions and, as such, is an invaluable source of information. The first manuscript titled “Factors influencing the pharmacological management of osteoporosis after fragility fracture: results from the Ontario Osteoporosis Strategy’s fracture clinic screening program” was published in Osteoporosis International. The lead author of the study, Dr. Dorcas Beaton, found that patient perceptions were pivotal in the path to initiating osteoporosis pharmacotherapy. Undergoing a bone mineral density (BMD) test was not as important as the patient understanding their test results. Knowledge of bone health and osteoporosis was also found to be important for post-fracture osteoporosis management.
The study concluded that interventions to facilitate accurate patient perceptions of BMD test and osteoporosis risk status could help improve osteoporosis treatment initiation rates. Rebeka Sujic was the lead author of the second study which examined factors predictive of the perceived osteoporosis-fracture link in fragility fracture patients. This study, published in the journal
Maturitas, found that most patients did not associate their fracture with their bone health even after a post-fracture intervention. At baseline (time of screening), 93% of patients did not believe that their fracture could have been caused by osteoporosis. Of these, only 8.2% changed this perception at follow up. This study also identified baseline factors associated with patients at a higher risk for not making the osteoporosis-fracture link at follow up: those who did not have a previous fragility, those who perceived their bones as “normal”, those who perceived fewer or no benefits to osteoporosis pharmacotherapy and those without a diagnosis of rheumatoid arthritis. Surprisingly, factors such as gender, age and osteoporosis knowledge were not found to be associated with making the osteoporosis-fracture link at follow up.
The study concluded that future post-fracture interventions should target patients at high risk for not making an osteoporosis-fracture link, emphasizing and personalizing the link between a fragility fracture and bone health, delivering a clear message about the quality of patient’s bones and discussing the benefits and risks of osteoporosis pharmacotherapy. The findings from these studies will be incorporated in post-fracture osteoporosis interventions to communicate to patients their risk for future fractures and osteoporosis with a final goal of helping improve the rates of osteoporosis management.
The risk of suffering a second spine fracture within the year following the first one is
0%
The FCSP is concentrating on creating tools and resources, such as an interactive, educational tool to assist patients with making the osteoporosis-fracture link.
0%
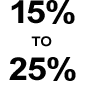
percent of all fractures in Canada after age 50 are caused by Osteoporosis.
Research Update
Research activities of the Fracture Clinic Screening Program
Testing – Working Group
In Ontario, in the absence of major restrictions to bone mineral density (BMD) testing, a sharp increase in BMD testing rates in much younger women, aged 40–44 years, for whom fracture risk is low, has been reported.1 In fiscal year 2007, BMD testing in women aged 40–59 years accounted for almost half (approximately 200,000) of all BMD tests performed.2 While this high rate of testing may indicate concern about osteoporosis as this age group approaches menopause, it also suggests unnecessary testing.
Evidence validates this suggestion; research by our group at Women’s College Hospital demonstrated that among healthy women age 40-60 years referred to a multidisciplinary osteoporosis clinic in Ontario for a baseline DXA test between 2005 and 2009, more than 90% had normal bone density.3
This study also showed that if a decision rule based on weight or menopausal status and fracture history was applied, then 33% of those who received the baseline BMD test would not have been recommended for testing.3 At the same time, clinical guidelines indicate women over 65 should be tested.4 Other research from our group has similarly demonstrated that reimbursement changes in 2008 in Ontario were associated with reduced testing rates among high risk individuals, notably those with recent fragility fractures.5 In 2010, about 12% of older men and 44% of older women (22% overall) who became eligible for DXA testing at age 65 years, were tested by age 70.6
Together, this evidence suggests that guidelines for BMD testing are not being followed. Previous research from our team demonstrated that, in a sample of BMD reports for fracture patients in Ontario, more than 50% of the time, reported fracture risks were misclassified by being underestimated (Allin 2013). Over 30% of reports containing a “low” fracture risk assessment should have been reported as “moderate” and over 20% of reports containing a “moderate” fracture risk should have been reported as “high” given the true fracture history.7 This has implications in terms of fracture risk categorization that can negatively affect subsequent follow-up care and treatment as current guidelines recommend that patients with high fracture risk be treated with bone-sparing agents.8
We have developed a standardized requisition for BMD referral or a Required Use Requisition (RUR) that aims to fill these care gaps by promoting appropriate referral and ensuring that the clinical risk factors that impact fracture risk assessment are available to the reading specialist at the time reporting.
The initial design of the RUR was created by the Ontario BMD Working Group, a committee composed of family physicians, radiologists, a BMD technician, and specialists with expertise in osteoporosis with representation from the Canadian Association of Radiologists, the Ministry of Health and Long-term Care, Osteoporosis Canada, and the Ontario College of Family Physicians and by Drs. Jaglal and Hawker.
The first version sought principally to communicate the best evidence surrounding baseline referral of low risk women.3 Subsequent interviews with family physicians revealed the need to communicate guidelines more broadly; guidelines for repeat testing and the relationship of guidelines to insurance policies were found to be particularly unclear.9 The RUR has been further refined based on consultation with developers of standardized forms currently in use in Manitoba, British Columbia, and Nova Scotia. Interviews with these stakeholders in addition to reading specialists have illustrated the potential for forms to communicate clinical details more accurately than patient self-reports, which are prone to error. Several major diagnostic imaging centres that perform BMD testing in the Greater Toronto Area have reviewed and verified that the RUR is acceptable to them. Before widespread implementation of the RUR can occur, our team would like to evaluate the effectiveness of the RUR. To do this, in September 2013, we submitted a grant proposal to the Canadian Institutes of Health Research to conduct a cluster randomized controlled trial.
There is also ongoing pilot testing of the RUR at Women’s College Hospital and clinics affiliated with the Scarborough Hospital as part of a post-graduate family medicine residents’ research project. At these locations, a hard copy of the RUR is being used by approximately 30 Ontario family physicians to further elucidate barriers to implementation and data collection for the trial.
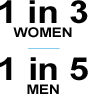
will suffer from an osteoporotic fracture during their lifetime
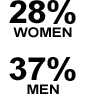
will suffer from an osteoporotic fracture during their lifetime
of hip fracture patients require admission to a nursing home
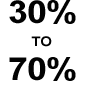
Several effective medications can reduce fracture risk by 30-70%
 Bone Fit™ 1-day workshop is aimed at the exercise and fitness professionals providing exercise programming in the community. The training provides foundational training to work safely in providing exercise training and programming to clients with low bone mass and uncomplicated osteoporosis. A special focus of this course is how to identify when a client should be referred to a physiotherapist.
Bone Fit™ 1-day workshop is aimed at the exercise and fitness professionals providing exercise programming in the community. The training provides foundational training to work safely in providing exercise training and programming to clients with low bone mass and uncomplicated osteoporosis. A special focus of this course is how to identify when a client should be referred to a physiotherapist.
The Bone Fit™ 2-day workshop is a comprehensive training program for rehabilitation professionals who work in a clinical environment where exercise prescription is the predominant modality for rehabilitation for clients with osteoporosis. The overall objective of this workshop is to provide grounding for safe clinical assessment and management of clients with osteoporosis through exercise-based rehabilitation.
More information on upcoming workshops and location of Bone Fit certified professionals can be found at www.bonefit.ca.
Award Recipient – A Champion for the Cause!
Osteoporosis Canada is proud to announce Dr. Earl Bogoch as the 2013 Lindy Fraser Memorial Award recipient. This prestigious award, established in 1993, recognizes an individual who has made an outstanding contribution to the field of osteoporosis research and education in Canada. The recipient is nominated by members of Osteoporosis Canada’s Scientific Advisory Council.
On Saturday Oct. 5th 2013, the 2013 Lindy Fraser Memorial Award was presented to Dr. Earl Bogoch at the annual OC SAC ASBMR Breakfast meeting in Baltimore. Osteoporosis Canada would like to congratulate Dr. Bogoch!
Osteoporosis Canada established this award in 1993. This prestigious award recognizes individuals who have done exemplary research and have helped to increase the knowledge about osteoporosis. The recipient is nominated by members of our Scientific Advisory Council.
Dr. Bogoch is an Orthopaedic Surgeon at St. Michael’s Hospital, and a Professor of Surgery at the University of Toronto, whose surgical interests have focused on surgical management of inflammatory arthritis, and hip and knee reconstruction. His interest in bone remodelling and structure lead him in the last fifteen years to the common orthopaedic issue of the fragility fracture patient who presents in clinic or hospital wards with increased, but usually unrecognized risk of future hip and vertebral fracture.
He has collaborated with scientists and program designers both in Canada and internationally to build system wide networks to identify and treat the high risk fragility fracture patient. After starting a small QI project at Wellesley Hospital, he formed a team at St. Michael’s Hospital with scientists, clinicians and a program manager to create a working coordinator model of systematic intervention for the fracture clinic and orthopaedic ward, where high risk fragility fracture patients are concentrated.
This team has worked with Osteoporosis Canada and others in seeking and obtaining support for and helping to develop, evaluate and improve a multicentre Ontario Program for fracture clinics.
With his colleagues, he has published and lectured widely on this subject and has promoted fracture prevention internationally. Research to optimize various aspects of the model has been widely published by the team. Efforts to promote models of systematic fracture prevention nationally and internationally have resulted in Dr. Bogoch working on projects involving numerous organisations such as the Canadian and Ontario Orthopaedic Associations, Osteoporosis Canada, Fraser Health Authority, International Osteoporosis Foundation, American Society of Bone and Mineral Research, Fragility Fracture Network, and the American Orthopaedic Association. Congratulations!
To learn more about Dr. Bogoch, please click on the link:
http://www.osteoporosis.ca/health-care-professionals/scientific-advisory-council/earl-r-bogoch/
Osteoporosis Long-Term Care
Osteoporosis Canada is proud to announce Dr. Earl Bogoch as the 2013 Lindy Fraser Memorial Award recipient. This prestigious award, established in 1993, recognizes an individual who has made an outstanding contribution to the field of osteoporosis research and education in Canada. The recipient is nominated by members of Osteoporosis Canada’s Scientific Advisory Council.
On Saturday Oct. 5th 2013, the 2013 Lindy Fraser Memorial Award was presented to Dr. Earl Bogoch at the annual OC SAC ASBMR Breakfast meeting in Baltimore. Osteoporosis Canada would like to congratulate Dr. Bogoch!
Osteoporosis Canada established this award in 1993. This prestigious award recognizes individuals who have done exemplary research and have helped to increase the knowledge about osteoporosis. The recipient is nominated by members of our Scientific Advisory Council.